Think of naloxone training like CPR or first aid. It’s a fundamental, life-saving skill that turns everyday people into first responders when it matters most. With the ongoing opioid crisis, knowing how to use naloxone is no longer a niche skill for medical professionals. This training gives you the confidence and the know-how to act when every single second counts.
Why Naloxone Training Is a Skill Everyone Needs
The opioid crisis continues to impact communities everywhere, making overdose a tragic but often preventable cause of death. This isn't just some abstract headline; it's a reality playing out in our neighborhoods, workplaces, and public spaces. The problem often boils down to a lack of immediate, on-the-scene help.
That’s where you come in.
Giving bystanders the right knowledge is the single most effective way to build a community-wide safety net. Naloxone training bridges the critical gap between the moment an overdose happens and when professional medical help can get there. It’s about transforming that feeling of helplessness into confident, decisive action.
The Growing Need for Trained Responders
The sheer scale of the opioid epidemic has driven a massive demand for naloxone. The market for this life-saving drug was valued at over USD 1.4 billion in 2025 and is projected to nearly double by 2032. This growth isn't just some business trend; it highlights a critical public health emergency.
Globally, drug use leads to about 500,000 deaths each year, with over 70% of those overdose fatalities directly linked to opioids. These numbers underscore a simple, powerful truth: the more people trained to use naloxone, the more lives we can save. Your decision to get trained directly contributes to a stronger, more resilient community.
Understanding the Root Cause
To truly grasp why naloxone training is so urgent, it helps to understand the complexities of opioid dependence and how it affects individuals, families, and entire communities. This context is vital for recognizing why intervention is so incredibly important.
Here’s a quick overview of the essential skills you'll gain from a typical naloxone training course.
What You Will Learn in Naloxone Training
Training ComponentKey TakeawayRecognizing Overdose SignsYou'll learn to confidently spot the key symptoms, like slow breathing, pinpoint pupils, and unresponsiveness.Administering NaloxoneYou'll get hands-on practice using common devices like nasal sprays (e.g., Narcan) and auto-injectors.Emergency Response StepsYou'll know the exact steps to take, from calling 911 to providing follow-up care after giving naloxone.Legal ProtectionsYou'll learn about Good Samaritan laws that legally protect you when you step in to help someone.
Mastering these skills ensures you’re not just a bystander, but an effective first responder ready to make a life-or-death difference.
How Naloxone Reverses an Opioid Overdose
To really get how naloxone works, it helps to picture the brain's opioid receptors as a bunch of parking spots. When someone takes an opioid like heroin or fentanyl, the drug molecules "park" in these spots. This is what produces the drug's effects, but it also leads to dangerous side effects like severely slowed or stopped breathing. During an overdose, all these parking spots are full, and the brain's control center for breathing basically shuts down.
Naloxone is what we call an opioid antagonist. All that means is it has a much stronger attraction—or affinity—to those same opioid receptors.

When you give someone naloxone, it’s like a priority tow truck with a master key. It rushes to those occupied parking spots, forcefully kicks the opioid molecules out, and takes their place. Once naloxone is parked in the receptors, it blocks the opioids from having any effect. This allows the person’s central nervous system to get back to its job—most importantly, breathing.
Its Role as a Rescue Drug, Not a Cure
It’s absolutely critical to understand that naloxone is an emergency antidote, not a treatment for addiction. Its effects are temporary, usually lasting between 30 to 90 minutes. This is a big deal because many opioids last much longer. When the naloxone wears off, the person can easily slip back into an overdose.
Calling 911 is always the most important step. Naloxone is a bridge to professional medical care, not a replacement for it. The person needs immediate medical attention to ensure their safety.
Common Forms of Naloxone
You’ll probably hear the brand name "Narcan" a lot, but naloxone comes in a few different, easy-to-use forms. Learning how to use these devices is a core part of any naloxone training program.
- Nasal Sprays: This is the most common form you'll find in community kits. It's a pre-filled, needle-free device that you simply spray into one nostril.
- Auto-Injectors: Think of an EpiPen. These devices give you verbal instructions and are designed to be pressed against the outer thigh to deliver a dose of naloxone.
One of the most incredible things about naloxone is how safe it is. If you give it to someone who hasn't taken opioids, it will have no effect. This makes it an incredibly safe tool to use even if you only suspect an overdose. Getting the right training is key, and it often goes hand-in-hand with other life-saving skills. You can learn more about combining this knowledge with other emergency skills in our guide to workplace CPR and naloxone training.
How to Recognize an Opioid Overdose
Knowing how to use naloxone is one thing, but that skill is only valuable if you can spot the emergency in the first place. The first and most critical step in saving a life is being able to confidently recognize the signs of an opioid overdose. It’s a high-stakes moment, and it's easy to second-guess yourself—is the person just deeply asleep, or are they in serious trouble?
This is exactly where naloxone training cuts through the confusion. It arms you with the knowledge to stop guessing and start looking for a specific cluster of symptoms that scream "medical emergency." While one or two signs might be easy to dismiss, seeing them all together is a clear and urgent call to action.

The Overdose Triad
In the medical world, professionals often look for what's known as the "opioid overdose triad." This isn't some complicated medical jargon you need to memorize. Think of it as a simple, three-point checklist to run through when you first assess the situation.
These are the three classic signs:
- Pinpoint Pupils: Take a look at their eyes. The black center part will shrink down to be incredibly small, sometimes described as the size of a pinhead.
- Slowed or Stopped Breathing: This is the most dangerous sign of all. Their breathing might be very shallow and slow, erratic, or it may have stopped entirely.
- Unconsciousness or Unresponsiveness: The person can't be woken up. You can shout their name or give them a firm shake on the shoulder, but they won't respond.
If you see these three signs together, you need to assume it’s an overdose and act immediately. Don't waste precious seconds debating what could be happening. Your number one priority is to get them breathing again.
Beyond the Triad: Other Critical Warning Signs
While that three-point triad is a powerful indicator, other physical signs can help confirm your suspicions. When someone overdoses, their body is starved of oxygen, and that causes very noticeable changes in how they look and sound.
Remember this simple rule: If they won’t wake up, call for help. You cannot harm someone by giving them naloxone if they don't have opioids in their system, but you can save their life if they do.
Keep an eye out for these additional red flags:
- Limp Body: Their muscles will be completely slack. The body will feel heavy and floppy, with no tension.
- Pale, Clammy Skin: Their skin may feel cool and damp to the touch.
- Blue or Grayish Tint: Check their fingernails and lips. A blueish or purplish color (called cyanosis) is a clear sign of severe oxygen deprivation. For people with darker skin, this might look more grayish or ashen.
- Choking or Gurgling Sounds: You might hear deep, snoring-like gurgles or choking noises. Sometimes called the "death rattle," these sounds mean the airway is blocked and the person is struggling for every breath.
Understanding these signs takes the guesswork out of a chaotic and stressful situation. When you can quickly and accurately figure out what's happening, you’re empowered to take the right steps without hesitation: call 911, give naloxone, and provide support until help arrives.
Your Step-by-Step Guide to Administering Naloxone
When you suspect an overdose, every second feels like an eternity. Having a clear, simple action plan is crucial. Your naloxone training is designed to help you stay focused and follow a specific sequence of steps that can make all the difference. This isn't about complicated medical procedures; it's about quick, effective actions you can take right now.
Think of it as your emergency checklist. In a high-stress moment, the last thing you want is to be guessing what to do next. The steps are designed to be easy to remember and straightforward to execute.
The Immediate Action Plan
Your response needs to follow a clear order. First, assess the situation and get professional help on the way. Then, you'll administer the life-saving medication.
- Check and Call: Shout the person’s name and give their shoulder a firm shake. If they don't respond, call 911 immediately. Put your phone on speaker so you can follow dispatcher instructions while keeping your hands free. Be sure to tell them you suspect an opioid overdose and that you have naloxone.
- Administer Naloxone: Give the first dose exactly as you were taught in your training. We'll break down the specific steps for both nasal sprays and auto-injectors in just a moment.
- Support Breathing: If you’re trained in rescue breathing and it’s needed, now is the time to start. An overdose stops breathing, so restoring oxygen is a top priority.
- Monitor and Repeat: Stay with the person. If they haven't started to respond after 2-3 minutes, it's time to administer a second dose of naloxone. Continue to monitor them until medical professionals arrive.
This simple infographic helps visualize the core process, breaking it down into three essential actions.
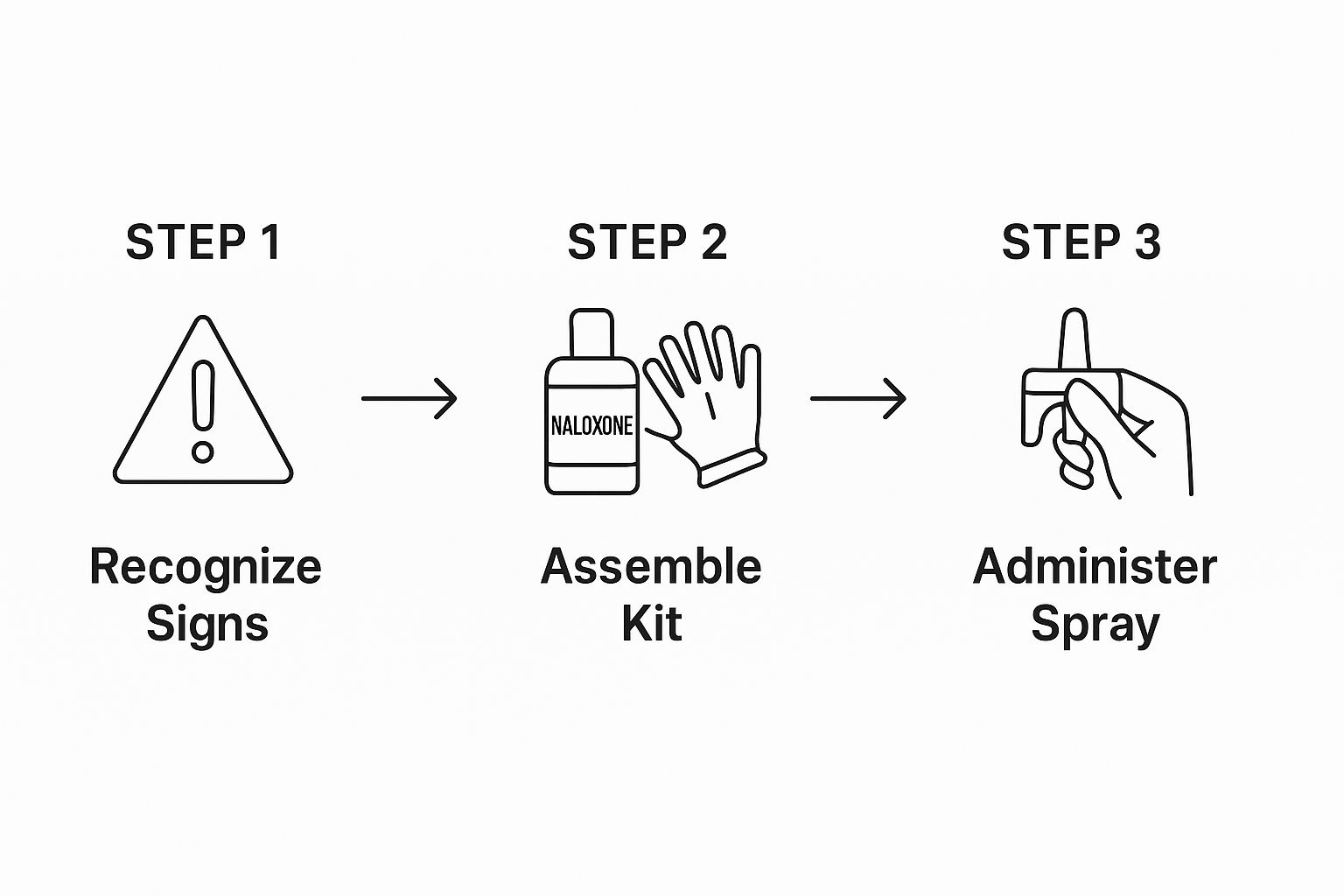
This flow highlights the simple, critical path from recognizing the emergency to taking life-saving action.
How to Use Naloxone Nasal Spray
Naloxone nasal spray, often known by the brand name Narcan, is the most common form you'll find available to the public. It’s designed so that anyone can use it with just a few simple steps.
- Peel back the package to take out the device.
- Hold the device with your thumb on the bottom of the plunger and your first and middle fingers on either side of the nozzle.
- Tilt the person’s head back and provide support under their neck to keep their airway open.
- Gently insert the tip of the nozzle into one nostril until your fingers touch the bottom of their nose.
- Press the plunger firmly to give the full dose of spray.
You don't need to prime or test the spray. It only contains one dose, so make sure you press the plunger all the way.
Crucial Reminder: Naloxone's effects are temporary, often lasting only 30 to 90 minutes. Many opioids last much longer. Calling 911 is non-negotiable because the person can slip back into an overdose once the naloxone wears off.
This kind of life-saving knowledge is incredibly empowering. Many people who master one emergency response skill feel inspired to expand their abilities even further. For those interested in teaching others, learning how to start a CPR training company can be a rewarding and impactful next step.
The Real-World Impact of Getting Trained
So, what kind of difference does naloxone training actually make? It’s not just about learning a new skill in a classroom. It’s about completely changing how someone acts in a real-life crisis. The proof is in the results: training transforms fear and hesitation into confidence and decisive action.
When more people in a community have this knowledge, they form a powerful safety net. This leads to faster responses and, most importantly, more lives saved.

Making the shift from a bystander to a first responder is a profound experience. Instead of feeling helpless, you're empowered to step in when a life is literally on the line. That empowerment creates a ripple effect, building a more resilient and prepared community one person at a time.
From Unsure to Unstoppable
One of the biggest obstacles in an overdose emergency is a person’s own confidence—or lack thereof. Without training, it’s completely natural to feel uncertain and second-guess yourself. With training, that uncertainty is replaced by a clear, step-by-step plan you know you can execute. The impact of this shift is measurable, and frankly, it's impressive.
Take training programs aimed at high-risk environments like the construction industry. In recent sessions, the number of participants willing to carry naloxone jumped from just 16% to over 80% after the course. Even more telling, confidence in responding to an overdose surged, with more than 80% feeling very confident post-training—a huge leap from the less than half who felt that way before. (Source)
Your decision to get trained isn't just about personal knowledge. It’s a tangible, positive contribution to the well-being of everyone around you—your family, your coworkers, and your neighbors.
A Community-Wide Safety Net
Think of each trained person as a single point of light in a network. By itself, one light is helpful. But when thousands of lights turn on across a city or workplace, they illuminate everything, leaving no one in the dark. This is exactly what happens when naloxone training becomes widespread. It creates a robust, community-wide safety net.
This principle is the same as the need for CPR training in the workplace; the more people who are trained, the stronger the chain of survival becomes for everyone.
This safety net has several key benefits:
- Faster Response Times: A trained individual on the scene can act immediately, bridging that crucial gap before paramedics arrive.
- Reduced Stigma: Widespread training helps normalize overdose response, treating it as the public health issue it is rather than something to be ignored.
- More Lives Saved: At the end of the day, more trained citizens lead directly to fewer preventable deaths.
Getting trained is a small investment of your time that pays enormous dividends for the entire community.
How to Find a Naloxone Training Course Near You
So you're ready to get certified in naloxone administration. That’s a fantastic decision, and getting started is probably easier than you think. The first step is simply finding a credible naloxone training provider, and you have some great options depending on how you learn best and what your schedule looks like.
Some people really thrive in a hands-on, in-person workshop. Others need the flexibility of an online course to fit training into their busy lives.
Your best bet is often to start local. Look for certified companies in your area, like Ready Response, that offer professional, hands-on training from experienced instructors. It's also a great idea to check with your local health department or community non-profits. They frequently host free or low-cost training sessions for the public.
Choosing the Right Training Format
Deciding between an online class and an in-person workshop usually comes down to personal preference and what works for you. Here’s a quick breakdown to help you figure it out:
- In-Person Training: This is the classic, hands-on approach. You get to practice with training devices and can ask your instructor questions right then and there. If you're a "learn by doing" person, this is for you.
- Online Training: The biggest advantage here is flexibility. You can learn at your own pace, from practically anywhere. It's a lifesaver if you have a packed or unpredictable schedule.
- Blended (Hybrid) Training: This format gives you the best of both worlds. You'll complete the learning portion online and then attend a brief, in-person session to practice your skills. It’s a nice balance of convenience and real-world practice.
No matter which format you pick, make sure the course provides a certification when you're done. This is your proof that you’ve gained the skills needed to act confidently and correctly in an emergency.
Expanding access to both naloxone and the training to use it is a critical public health strategy for reducing overdose deaths. Efforts from organizations like the Clinton Foundation have already helped deploy over 846,000 doses to communities across the country. This highlights the incredible momentum behind this movement. You can read more about why 2025 is seen as a critical year in the fight against overdose deaths.
This kind of training is a perfect complement to other life-saving skills. If you're building a solid foundation of emergency response knowledge, you might also want to look into getting your CPR and AED certification.
Frequently Asked Questions About Naloxone
It’s completely normal to have a lot of questions before, during, and even after your naloxone training. Stepping up to save a life is a big deal, and getting clear, direct answers is what builds the confidence you need to act without hesitation. Let's tackle some of the most common questions we hear.
Can I Get in Trouble for Helping Someone?
This is probably the biggest worry we hear, and it's a valid concern. The good news is the answer is almost always no. Every single state has a form of Good Samaritan Law that gives legal protection to people who act in good faith to help someone who is ill, injured, or in danger.
These laws were specifically created to encourage everyday people like you to help in an emergency without fearing a lawsuit. When it comes to an overdose, these laws protect you when you call 911 and administer naloxone.
What Happens After I Give Someone Naloxone?
Naloxone is incredibly effective, working fast to reverse an opioid's effects. But because it works so quickly, it can push the person into immediate withdrawal. When they wake up, they might be confused, sick, or agitated.
The most important thing to remember is that naloxone is temporary. It wears off in 30-90 minutes. You must stay with the person until professional medical help arrives, because the overdose can return once the naloxone wears off.
How Should I Store My Naloxone Kit?
Proper storage is simple but critical. If you don't store your kit correctly, it might not work when you need it most. Just think of it like any other important medication:
- Temperature: Keep it at room temperature. Don't leave it in a hot car in July or a freezing one in January, as extreme temperatures can ruin it.
- Light: Store it out of direct sunlight.
- Expiration: Check the expiration date every so often and get a new kit if it's expired.
Is This the Only Thing I Will Learn?
While the main event is learning how to use naloxone, any good training course covers much more. You'll learn the entire emergency response process—from spotting the signs of an overdose to making the call to 911 and providing supportive care until help arrives. Many people find this training is a perfect partner to other skills like CPR and first aid.
If you have other questions about our specific programs, we’ve answered a lot more on our FAQs page.
At Ready Response, we provide hands-on, expert-led naloxone training that gives you the skills and confidence to save a life. Learn more about our courses and get certified.
SEO Title: Naloxone Training: Your Complete Guide to Saving a Life
Meta Description: Get certified with our complete guide to naloxone training. Learn to recognize an overdose, administer Narcan, and save a life with confidence.
