When an adult suddenly collapses, your first moves are the most critical ones you can make. It all starts with a few straightforward checks: first, make sure the scene is safe, then check if the person is responsive and breathing. If they're unresponsive and not breathing normally, your next two steps are to call 911 immediately and then get started on chest compressions.
First Steps in a Cardiac Emergency

When you witness a cardiac emergency, hesitation is the enemy. Seriously. The clock starts ticking the second someone goes down, and how you respond in those initial moments can completely change the outcome. Before you even think about starting compressions, your first job is to ensure the scene is safe for everyone—including you.
Take a quick scan of your surroundings. Are there any immediate dangers like downed power lines, oncoming traffic, or spilled chemicals? The golden rule here is that you can't help anyone if you become a victim, too. Your safety comes first, always.
Check, Call, and Get Help
Once you've confirmed it's safe to approach, your focus shifts to the person. Kneel beside them and give their shoulder a firm tap. Shout something direct and clear, like, "Are you okay? Can you hear me?"
At the same time, look at their chest for signs of normal breathing. Give this a solid 5 to 10 seconds. It's super important not to mistake agonal gasps for actual breathing—these look more like sporadic, fish-out-of-water gasping or snoring sounds and are a dead giveaway for cardiac arrest.
If you get no response and see no normal breathing, it's go-time.
A quick reference can be a lifesaver when your adrenaline is pumping. Here’s a simple table to guide your first 30 seconds.
Your First 30 Seconds in an Emergency
With these critical first actions out of the way, you can move on to providing direct care with confidence, knowing that professional help has been activated.
The statistics are sobering: survival from an out-of-hospital cardiac arrest can be as low as 12%. However, immediate CPR can double or even triple a person's chance of survival.
It's also important to consider why the person is unresponsive. If you suspect they might be choking, the approach is different. For that specific scenario, check out our detailed guide on how to help someone choking.
By quickly securing the scene and getting emergency services on the way, you’ve set the stage for effective life support.
Delivering High-Quality Chest Compressions
Once you’ve confirmed the person needs help and that 911 is on the way, your immediate focus shifts to chest compressions. This is the absolute core of CPR. Effective compressions aren't just about pushing on the chest—they're about physically pumping the heart to get oxygen-rich blood circulating to the brain and other vital organs.
The quality of your compressions has a direct, massive impact on the person’s chance of survival. Don't think of it as a frantic emergency procedure, but more like a physical task that demands good technique to actually work.
Perfecting Your Hand Placement and Body Mechanics
First things first, get into the right position. Kneel right beside the person’s chest. Find the center of their breastbone (the sternum), which is usually in line with the nipples, and place the heel of one hand there.
Put your other hand directly on top of the first and interlock your fingers. Pull your fingers up so they aren't touching the chest—this little trick helps focus all the pressure through the heels of your hands where it's needed most.
With your arms straight and elbows locked, position your shoulders directly over your hands. You’re not trying to push with your arm muscles; you’re using your entire upper body weight. This technique is the key to delivering powerful, consistent compressions without getting exhausted in the first minute.
A common mistake I see in classes is people bending their elbows. This forces you to rely on your weaker bicep and tricep muscles. By keeping your arms straight and pivoting from your hips, you let gravity do most of the work for you. It's a game-changer.
Finding the Right Rate and Depth
Now, let's talk about rhythm. It's just as important as your hand placement. You need to push at a steady rate of 100 to 120 compressions per minute. If you need a mental metronome, the beat of the song "Stayin' Alive" by the Bee Gees is the perfect tempo to keep in mind.
Each push needs to be deep enough, compressing the chest about 2 inches, but no more than 2.4 inches.
Just as crucial as the push is the release. After every single compression, you have to let the chest fully recoil, or return to its normal position. This recoil is what allows the heart's chambers to refill with blood before you push again. Without it, you're just pushing on an empty pump. If you want to dive deeper into this, we have a whole guide on the ideal CPR chest compression rate.
Here’s a quick visual reminder of the initial emergency steps that lead up to performing these life-saving compressions.
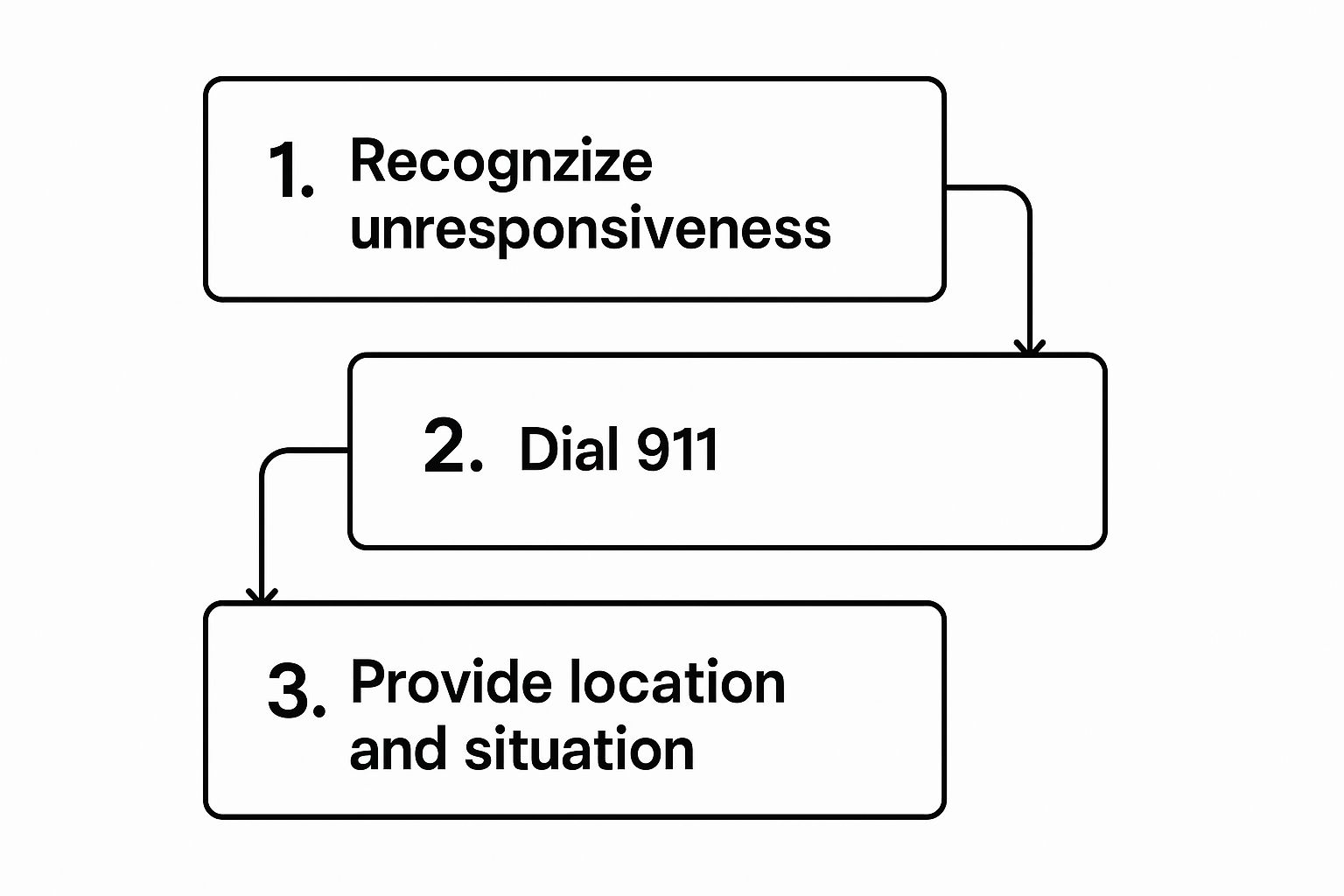
This simple flow—recognize, call, and inform—is what kicks everything off, ensuring professional help is dispatched while you begin the critical work of compressions. Time is everything. Recent data highlights that when a bystander starts CPR within the first few minutes, survival rates can jump dramatically.
Performing Rescue Breaths With Confidence

After you've delivered 30 solid chest compressions, it’s time to get some oxygen into the person’s system. While compressions are absolutely the priority, rescue breaths are a crucial part of the cpr steps for adults, especially if the cardiac arrest has gone on for more than a few minutes. Your goal is simple: get air into the lungs so the compressions can push that oxygenated blood to the brain and other vital organs.
The first hurdle is making sure the airway is actually open. When someone is unconscious, their tongue can relax and fall back, blocking the throat. The go-to method for clearing this is the head-tilt, chin-lift maneuver—it's fast, simple, and incredibly effective.
Just place one hand on their forehead and gently tilt the head back. Use the fingertips of your other hand to lift the chin from its bony part. This simple movement pulls the tongue forward and opens up a clear path for air.
Delivering Effective Breaths
With the airway open, you’re set to give two breaths. If you have a CPR barrier device, like a pocket mask, now is the time to use it. It’s always a good idea to create a safe barrier between you and the person you're helping.
Pinch the person's nose closed so the air you give doesn't just escape. Then, make a complete seal over their mouth with your mouth or the mask.
Important Tip: You don't need to deliver a huge, forceful gust of air. A breath that lasts about one second and is just strong enough to make the chest visibly rise is perfect. Think of it as a normal breath, not a deep one.
Give the first breath and watch the chest rise. Let it fall back down naturally, and then deliver the second one. The whole process of giving two breaths needs to happen in less than 10 seconds. Minimizing the pause in chest compressions is critical.
- Breath 1: Watch for a gentle, visible chest rise.
- Pause: Allow the chest to fall completely.
- Breath 2: Give the second breath, again looking for that chest rise.
What if the chest doesn't rise? Don't panic. It happens. Just reposition the head with another head-tilt, chin-lift and try giving a breath one more time. If it still doesn’t go in, don't waste any more precious seconds on it. Go right back to chest compressions. Keeping that blood circulating is the most important thing you can do.
How to Use an AED with CPR
While chest compressions and rescue breaths are your primary tools for keeping blood flowing, an Automated External Defibrillator (AED) is what can actually fix the underlying problem. Think of it as a controlled reboot for the heart’s chaotic electrical system during a sudden cardiac arrest.
The great thing is, these devices are specifically designed for anyone to use, even without a medical background. When an AED arrives on the scene, the very first thing you do is power it on. It will immediately start talking you through every single step with clear, calm instructions. Don't stress about remembering a complicated sequence; just listen and follow its lead.
Applying the Pads and Following Prompts
Once the AED is on, its first instruction will be to expose the person's chest. You’ll need to remove clothing to apply the pads directly to the bare skin.
Open the pad package. The pads themselves have simple diagrams showing exactly where they need to go—one on the upper right side of the chest and the other on the lower left side, just below the armpit. Getting this placement right is critical because it ensures the electrical current can pass through the heart effectively. You can learn more by checking out our guide on the key factors for effective AED pad use.
With the pads firmly in place, plug the connector into the AED if it isn't already. The machine will then announce that it's analyzing the heart's rhythm.
Crucial Safety Moment: The AED will audibly warn, "Do not touch the patient." This is non-negotiable. It is absolutely vital that you and everyone else stands clear. If a shock is delivered while someone is in contact, the electricity can travel right through them, too.
If the AED determines a shock is necessary, it will begin to charge and then instruct you to press the flashing "shock" button. When you press it, the person's body may jolt, which is a completely normal reaction to the electrical impulse.
What happens next is just as important. Do not wait for further instructions. As soon as the shock is delivered, get right back on the chest and resume compressions immediately. The combination of an electrical shock followed by high-quality CPR gives the person the absolute best chance of survival.
Navigating the Moments Until Help Arrives

You’ve started CPR. Now what? Those minutes before paramedics show up can feel like an eternity, but this is where your efforts truly matter. Your only job right now is to keep those compressions going strong. Effective, non-stop compressions are what give this person their best shot.
But let's be realistic—performing high-quality CPR is exhausting work. Rescuer fatigue is a very real, very significant factor. Even if you feel fine, the quality of your compressions can start to dip after just a couple of minutes.
This is where a partner comes in handy. If someone else is there, you should switch out every two minutes (that’s about five cycles of 30 compressions and 2 breaths). A smooth switch is key. The next person should be kneeling on the opposite side, ready to jump in the second you finish a cycle. This keeps the pause in compressions down to just a few seconds.
When to Stop or Change Your Actions
This is probably the most common question I get in my classes: "When do I get to stop?" It's a fair question, and the answer is only under very specific conditions. You should only stop CPR if:
- You see obvious signs of life. The person starts breathing on their own, moving, or opens their eyes.
- An AED is ready to use. You'll need to pause compressions so the device can analyze the heart's rhythm.
- Another trained person takes over. This is your chance to switch and fight off fatigue.
- Emergency medical services (EMS) arrive and take over. The paramedics will tell you when they’re ready to step in.
- You are physically too exhausted to continue. Your safety matters, too. Don't push yourself to the point of becoming a second patient.
It’s also crucial to have a realistic perspective on outcomes. A lot of people see CPR on TV and think survival rates are incredibly high. One study found that a staggering 90.7% of people overestimated survival chances. The reality is much more sobering. You can learn more by checking out the full study findings on CPR survival expectations.
The most important thing to remember is that you are the bridge to professional medical help. Your actions are giving this person a chance they would not have had otherwise. When EMS arrives, give them a quick, clear summary: what you saw, what you did, and for how long.
From Knowledge to Action with Formal CPR Training
Reading an article about the cpr steps for adults is a fantastic first step. Seriously. You now have a solid foundation of what to do in a cardiac emergency, which is more than most people can say.
But let's be real. When you're faced with a real crisis, adrenaline pumping and seconds counting, that theoretical knowledge can feel a million miles away. This is where professional, hands-on training becomes absolutely essential.
True readiness isn’t just about knowing the steps; it's about having the muscle memory and mental conditioning to perform them under immense pressure. Formal training is what bridges that critical gap.
Why Certification Builds Real Confidence
In a professional course, you move beyond just reading and into doing. You'll practice compressions on a responsive manikin that gives you real-time feedback on your rate and depth. You get to feel what proper hand placement is like and learn how to use your body weight effectively—skills that are impossible to truly grasp from a screen.
An instructor doesn't just teach the "what"; they show you the "how" and "why" in a way that sticks. They can correct your form instantly, answer your specific questions, and run you through scenarios that mimic the chaos of a genuine emergency.
This guided practice is what transforms knowledge into an instinctual, life-saving skill. If you're serious about being prepared, exploring options for getting your CPR and AED certification is the single most important next step you can take.
At Ready Response, our courses are designed to build that unshakable confidence. We believe everyone should feel empowered to act. Our hands-on training ensures that when the moment arrives, you won’t just know what to do—you’ll be ready to do it, making you a true and vital link in the chain of survival.
Still Have Questions About Adult CPR?
Even after you've learned the basics, it's completely normal for a few questions to pop up. Honestly, thinking through these "what-ifs" ahead of time is what builds the confidence you need to act without hesitation when it counts.
Can I Get in Trouble for Performing CPR?
Absolutely not. This is a big fear for a lot of people, but you can put it to rest. Good Samaritan laws exist in all 50 states to protect bystanders who step up in good faith to help someone during an emergency.
It's always, always better to do something than to do nothing. Think about it: in a true cardiac arrest, the alternative to CPR is certain death. Your actions can only help.
Is It True I Might Break Ribs?
Yes, this can happen. When you're performing deep chest compressions correctly, especially on an older adult, it’s possible for ribs to fracture.
But here’s the perspective you need: a broken rib is a treatable injury. A heart that isn’t beating is fatal. Don’t let this fear hold you back from pushing hard and fast. Your goal is to save a life.
Cardiac Arrest vs. Heart Attack: What’s the Difference?
This is probably one of the most common points of confusion, and the distinction is critical.
- Heart Attack: This is a "plumbing problem." A blockage is stopping blood flow to the heart. The person is usually awake, conscious, and breathing, though they will be in distress.
- Cardiac Arrest: This is an "electrical problem." The heart's electrical system malfunctions, and it suddenly stops beating altogether. The person will be unconscious and not breathing.
You only perform CPR for cardiac arrest.
For a more detailed look at common concerns, you can explore our full list of CPR FAQs.
At Ready Response, we turn your knowledge into life-saving skills. Our hands-on training builds the confidence to act when it matters most, ensuring you are prepared for any emergency. Find a class and get certified at https://readyresponsepa.com.
