When a burn happens, what you do in those first few moments is everything. The initial shock can make it hard to think straight, but having a clear plan can make a massive difference in the outcome. Your response in the first five minutes truly sets the stage for healing and can stop a minor injury from turning into something much worse.
Effective burn treatment first aid isn't complicated, but it has to start immediately. Your first priority is always to stop the burning process. After that, it's all about cooling the skin. Get this right, and you're already halfway there.
What to Do in the First Five Minutes of a Burn
Panic is a natural reaction, but a few calm, deliberate actions can dramatically improve the situation. Let's walk through the immediate steps.
Secure the Scene and Stop the Burn
First things first: safety. You have to stop the source of the burn immediately.
This means getting yourself or the injured person away from whatever caused it. If it’s a grease fire on the stove, move out of the kitchen. If it’s a chemical splash, you need to safely remove contaminated clothing without letting it touch other areas of skin. For electrical burns, the power source must be shut off before you even think about approaching the person.
It sounds obvious, but in a moment of distress, it's easy to forget. The main goal here is simple: prevent any more harm to the victim or to yourself.
Cool the Burn Correctly
Once everyone is safe, the single most important next step is to cool the burn down.
Place the burned area under cool—not icy cold—running water for a solid 10 to 20 minutes. I can't stress this enough. This isn't just a quick rinse. That extended time is crucial for pulling heat out of the deeper layers of skin and stopping the tissue damage from progressing.
A huge mistake people make is grabbing ice. Never apply ice directly to a burn. The extreme cold can cause frostbite and damage the already fragile skin even more. Just stick with cool tap water.
Globally, burns are a serious public health issue, leading to an estimated 180,000 deaths each year. Most of these injuries happen right at home or work—places where knowing proper first aid can literally be the difference between life and death. The right immediate care is proven to reduce the severity of burns and improve outcomes, as detailed in research published by the National Center for Biotechnology Information.
After you've finished cooling the burn, gently remove any tight clothing or jewelry near the affected area. Swelling can start surprisingly fast, and things like rings, watches, or bracelets can quickly become too tight and cut off circulation.
Be gentle. If any clothing is actually stuck to the burn, don't force it. Just cut around the fabric and leave the stuck part in place for a medical professional to handle.
How to Identify the Severity of a Burn
Not all burns are created equal. Knowing the difference is the first critical step in providing the right burn treatment first aid. Your immediate actions depend entirely on whether you're dealing with a minor burn you can handle at home or a serious injury that needs a doctor—fast. Assessing a burn is all about looking at its depth, how it appears, and how much it hurts.
Honestly, a quick assessment can tell you almost everything you need to know to make the right call. It’s simpler than you might think.
This visual guide breaks down the three main burn categories, showing which layers of skin are affected and the key signs to look for.
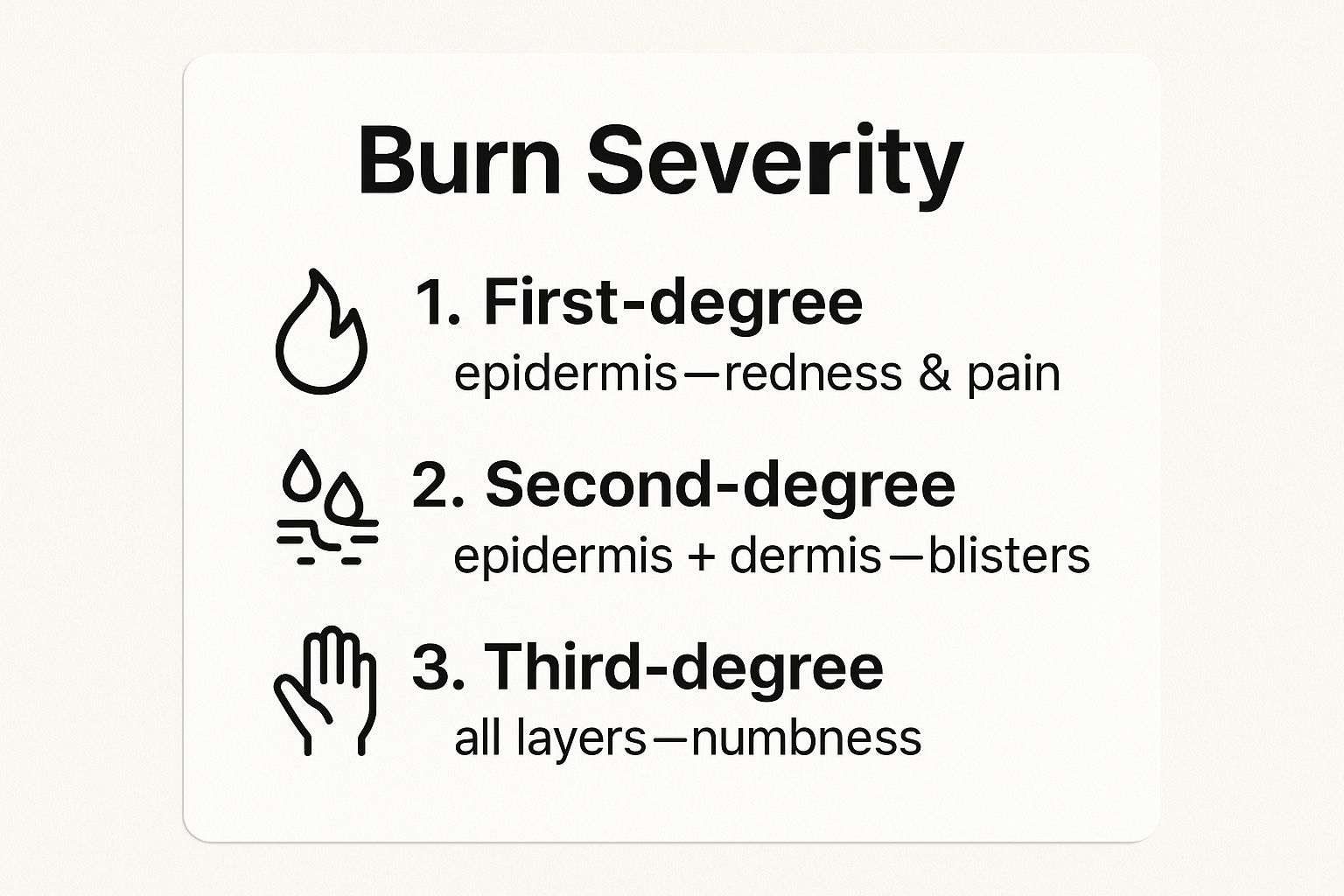
As you can see, the deeper the burn goes, the more severe it is. That's your cue that professional medical attention is needed.
Burn Severity at a Glance
Sometimes you need a quick reference to figure out what you're dealing with. This table breaks down the key differences between burn degrees to help you make a fast, accurate assessment in a stressful moment.
Looking at these side-by-side makes it clear how the signs change as the injury worsens. Remember these visuals—they're your best guide for what to do next.
First-Degree Burns: The Most Common Type
First-degree burns are superficial, only touching the outermost layer of skin, the epidermis. Think of a mild sunburn or accidentally brushing against a hot pan. The skin will look red, feel painful, and might be a little swollen, but you won't see any blisters.
These are the least severe burns and usually heal up on their own in about a week without leaving a scar. While they're definitely uncomfortable, they can almost always be treated effectively at home.
Second-Degree Burns: When Blisters Appear
Once a burn gets deeper and hits the second layer of skin (the dermis), it's classified as a second-degree burn. The dead giveaway? Blisters. The skin will also be intensely red, swollen, and might look blotchy.
These burns hurt a lot more than first-degree ones because the nerve endings are more exposed and irritated.
A key takeaway here is the presence of blisters. If you see them, you're looking at a second-degree burn. It needs more careful attention to prevent infection, and whatever you do, don't pop the blisters. They act as a natural, sterile bandage.
Small second-degree burns (less than three inches across) can sometimes be managed at home, but larger ones—or any on sensitive areas—need a doctor's evaluation. For more in-depth safety information, you can always explore the resources on the Ready Response blog.
Third-Degree Burns: A Sign of Deep Damage
Third-degree burns are the most severe and are always a medical emergency. They destroy both the epidermis and dermis and can even reach into the underlying fat, muscle, or bone.
You can't mistake the appearance of a third-degree burn. The skin might look:
- Waxy and white
- Charred or blackened
- Leathery or tough
- Dark brown
Here's the scary part: these burns might cause very little or even no pain. This is a dangerous sign. It means the nerve endings in the skin have been completely destroyed. Any third-degree burn requires an immediate 911 call.
Location and Size Matter, Too
Beyond the burn's depth, its size and location are just as important. Generally, any burn larger than the palm of your hand is considered major.
Also, any burn—no matter the degree—on these specific areas is a red flag that needs professional medical attention:
- Face or eyes
- Hands or feet
- Groin or buttocks
- Over a major joint, like a knee or shoulder
These parts of the body are functionally critical and are more prone to severe swelling, infection, and scarring that can lead to long-term problems.
Caring for Minor Burns at Home
Once you've cooled a minor burn and are sure it doesn't need a trip to the doctor, your focus shifts to healing. The goal is simple: create the best environment for your skin to repair itself. This all comes down to preventing infection and protecting the damaged area.
Think of it as keeping the burn clean, covered, and comfortable.

This process isn't complicated, but it's important to do it right. Skipping a step can open the door to infection or lead to more noticeable scarring. With the right approach, you can manage the healing process with confidence.
Gentle Cleaning and Application
After the initial cooling, the burn needs a very gentle cleaning. Use a mild soap and lukewarm water, then carefully pat the area dry with a clean cloth. Do not rub the skin. Rubbing can cause even more irritation and might break any small blisters that are forming.
With the area completely dry, go ahead and apply a thin layer of antibiotic ointment. This does a couple of important things:
- It creates a barrier against bacteria, helping to prevent infection.
- It keeps the wound moist, which can actually promote better healing.
Steer clear of old home remedies like butter, thick creams, or oils. These can trap heat right against the skin and introduce bacteria, making a minor problem much worse.
Dressing and Protecting the Burn
Covering the burn is a critical step. A good dressing protects the sensitive skin from the air, which can help reduce pain, and it also shields it from friction and germs.
Your best bet is a sterile, non-stick gauze pad. Avoid anything fluffy like cotton balls, as their fibers can get stuck in the wound and make healing a real headache. Secure the gauze loosely with medical tape.
You’ll want to change this dressing at least once a day, or more often if it gets dirty or wet. Each time you change it, just repeat the process: gently clean the area and reapply a thin layer of antibiotic ointment. Having the right first aid supplies makes this whole process much easier.
Managing Pain and Monitoring for Infection
Even a small burn can hurt quite a bit. Over-the-counter pain relievers like ibuprofen or acetaminophen are great for managing the discomfort and keeping inflammation down. Just be sure to follow the dosage instructions on the package.
It's a surprising fact, but most burn injuries—somewhere between 72 to 94 percent—actually happen right at home. Research consistently shows that getting first aid right from the start (like proper cooling and covering) makes a huge difference. It can reduce tissue damage, shorten hospital stays, and lower the overall cost of care. You can dive deeper into these findings on burn first aid awareness.
As the burn heals, keep a close eye on it for any signs of infection. If you start to see increased redness, swelling, pus, or notice a foul smell, it's time to call the doctor. A fever is another red flag that means you need professional medical attention.
Red Flags: When You Must See a Doctor
Knowing how to handle a minor burn at home is an essential skill, but it’s just as important to recognize when a burn is beyond your ability to treat. Hesitating to seek professional medical help can lead to serious complications like widespread infection, permanent scarring, or even loss of function.
Think of these red flags as non-negotiable signals to get to a doctor or emergency room right away.

This isn’t just about the obvious, severe third-degree burns. A handful of other factors can turn what looks like a manageable injury into a medical emergency. The best burn treatment first aid often means knowing exactly when to hand things over to a professional.
Location and Size Are Critical
Sometimes, the location of a burn is far more telling than its depth. A relatively small burn in the wrong place can be much more dangerous than a larger one on a less critical area, like your thigh.
You should always seek immediate medical care if a burn is on the:
- Face, hands, or feet: These spots have thin skin, are prone to swelling that can cut off circulation, and are functionally critical. Scarring here can lead to long-term mobility issues.
- Major joints: A burn over a knee, shoulder, elbow, or along the spine can cause the skin to tighten as it heals, which can severely limit your range of motion.
- Groin or buttocks: These sensitive areas are highly susceptible to infection simply because of where they are.
Beyond the burn's location, size is a major factor. As a general rule, if a second-degree burn is larger than three inches in diameter, it absolutely requires professional medical attention.
Specific Types of Burns That Demand Attention
Some burns are automatic emergencies, no matter how they look on the surface. That's because certain types can cause deep, hidden damage that isn’t immediately visible.
Any chemical or electrical burn requires an immediate trip to the emergency room. Chemical burns can continue to eat away at tissue long after the initial contact, while electrical burns can cause severe internal injuries to muscles, nerves, and even the heart—with minimal evidence on the skin.
This is where expert evaluation becomes essential. At Ready Response, our range of safety training services emphasizes the importance of recognizing these high-risk situations to ensure the best possible outcomes.
Warning Signs of Infection
Even a minor burn can spiral into a major problem if it gets infected. You'll need to keep a close eye on the healing process and watch for these tell-tale signs of trouble:
- Spreading redness that moves beyond the original burn area.
- Increased swelling or pain a few days after the injury.
- Pus or a yellowish/greenish discharge oozing from the wound.
- A foul odor coming from the burn.
- Fever or feeling generally unwell.
Any one of these symptoms means you need to see a doctor. An infection won't clear up on its own and requires medical intervention, usually antibiotics, to prevent it from spreading. Making the right call quickly is a crucial part of first aid.
Common Burn Treatment Mistakes to Avoid
In the heat of the moment, it’s easy to panic and fall back on old wives’ tales or gut reactions. But when you’re dealing with burn treatment first aid, what you don’t do is often just as critical as what you do.
Some of the most common "remedies" you've probably heard about can actually trap heat, introduce bacteria, and make the injury significantly worse. This isn't just an assumption; a widespread lack of adequate knowledge about burn first aid exists among the general public. You can explore more about these findings on burn first aid knowledge gaps to see why busting these myths is so important. Correct first aid can literally save skin.
The Problem with Greasy and Goopy "Fixes"
Let’s get this one out of the way immediately: never put butter, oil, toothpaste, or egg whites on a burn. It's a persistent myth, but these substances do way more harm than good.
Here's why:
- They Trap Heat: Instead of letting the skin cool, greasy substances create an insulating layer that holds heat in. You're essentially allowing the burn to continue cooking the tissue underneath.
- They Increase Infection Risk: These are not sterile products. Slathering them onto broken, compromised skin is like rolling out the welcome mat for bacteria, which can lead to a nasty infection.
The right move is always the simplest: cool, running water. That’s it. Nothing else should touch the burn until it’s been thoroughly cooled down.
Why You Must Avoid Ice and Icy Water
When something is hot, it seems logical to fight it with extreme cold. But applying ice directly to a burn is a major mistake. The intense cold can cause frostbite on skin that is already incredibly fragile and damaged.
This can lead to a second injury on top of the first, further damaging blood vessels and deepening the tissue trauma. Stick with cool tap water—it’s effective enough to stop the burning process without causing additional harm.
Having the right first aid kit supplies, like sterile non-stick dressings, is far more useful than anything you'll find in your freezer.
Leave Blisters Alone
Blisters are your body’s natural defense mechanism. Think of a blister as a sterile, fluid-filled bubble that acts as a biological bandage, protecting the delicate new skin underneath from air and bacteria.
Popping a blister intentionally tears this protective layer open. This exposes the raw, sensitive wound to infection and can absolutely increase pain and scarring.
As long as a blister is intact, just leave it be. If it happens to break on its own, gently clean the area with mild soap and water, apply an antibiotic ointment, and cover it with a sterile bandage.
Frequently Asked Questions About Burn First Aid
When you’re dealing with a burn, your mind can race with questions. It’s completely normal to feel uncertain, even after the initial crisis has passed. Let’s clear up some of the most common concerns people have with direct, practical answers to help you through the healing process.
Proper burn treatment first aid is more than just a few minutes of immediate care. Knowing the right follow-up steps is just as important as the first response.
How Long Should I Really Run Cool Water Over a Burn?
You need to aim for a solid 10 to 20 minutes under cool, running water. This isn't just about making it feel better; it actively stops the burning process deep within the skin's layers, which keeps the injury from getting worse.
If you cut this step short, the heat trapped in the skin can continue to cause damage long after you've moved away from the source. This extended cooling period is one of the single most effective things you can do for a minor burn. Just be sure to never use ice or ice-cold water, as the extreme temperature can cause even more tissue damage.
Is It Okay to Put Aloe Vera on a New Burn?
For a minor first-degree burn (think a mild sunburn), pure aloe vera gel can be wonderfully soothing, but there's a catch: only apply it after the burn has been properly cooled with running water for at least 10 minutes.
Putting anything on a burn before it's fully cooled can trap heat and make the injury worse. If the skin is broken in any way—like a popped blister—or if you're dealing with a more serious second or third-degree burn, skip the aloe entirely. Your focus should be on preventing infection, so it's best to consult a doctor.
What Are the Signs of an Infected Burn?
It’s crucial to keep a close eye on any burn in the days following the injury. Catching an infection early is key to preventing serious complications.
Here are the red flags to watch for:
- Increased pain that gets worse over time instead of better.
- Redness spreading out from the original burn area.
- Significant swelling around the wound.
- Yellowish or greenish pus or other fluid weeping from the wound.
- The area feeling noticeably warm to the touch.
- Running a fever.
If you spot any of these signs, don't wait it out. See a healthcare provider right away, as you'll likely need medical treatment like antibiotics.
Should I Cover a Burn or Let It Air Out?
This really depends on the type of burn you have. The main question is whether the skin is broken.
For simple, first-degree burns without any broken skin, leaving them uncovered is generally fine. But for second-degree burns with either intact or broken blisters, covering them is the best practice.
Use a sterile, non-stick bandage to shield the area from bacteria. This also helps reduce pain by keeping air off the exposed nerve endings. Make sure to change the dressing daily, or anytime it gets wet or dirty. Steer clear of fluffy materials like cotton balls, which can stick to the wound and leave fibers behind.
Having a solid understanding of first aid is invaluable. If you have more questions about first aid or safety protocols, you can find a wealth of information in the Ready Response FAQs section.
Being prepared to act confidently in an emergency is a skill that empowers you to protect yourself and those around you. At Ready Response LLC, we provide hands-on training that turns knowledge into life-saving action. Explore our first aid and CPR courses at https://readyresponsepa.com to gain the skills that truly matter.
